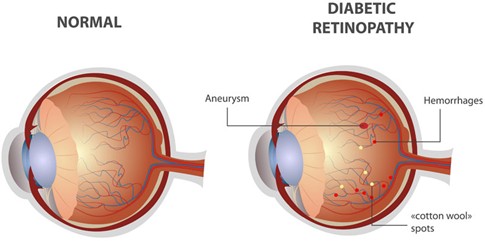
Diabetic retinopathy (DR) is a common and serious eye disease caused by long-standing diabetes mellitus. It affects the retina, the light-sensitive layer at the back of the eye, and is one of the leading causes of preventable blindness among working-age adults. Early detection and proper control of diabetes can prevent or delay vision loss.
What Is Diabetic Retinopathy?
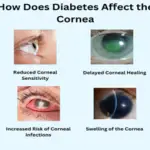
Diabetic retinopathy occurs due to damage to the small blood vessels of the retina as a result of persistently high blood sugar levels. Over time, these vessels become weak, leaky, or blocked, leading to retinal damage and impaired vision.
Causes and Risk Factors
Primary Cause
Chronic hyperglycemia (high blood sugar) causing microvascular damage
Major Risk Factors
Long duration of diabetes
Poor glycemic control
Hypertension
High cholesterol levels
Pregnancy
Kidney disease
Smoking
The risk and severity of diabetic retinopathy increase with the duration of diabetes, regardless of whether it is Type 1 or Type 2.
Pathogenesis (How It Develops)
Damage to retinal capillaries
Increased vascular permeability → fluid leakage
Capillary closure → retinal ischemia
Release of vascular growth factors (VEGF)
Formation of abnormal new blood vessels
Symptoms of Diabetic Retinopathy
Early Stage
Often asymptomatic
Mild blurring of vision
Difficulty with night vision
Advanced Stage
Floaters (black spots or strings)
Sudden loss of vision
Distorted or patchy vision
Difficulty reading or recognizing faces
⚠️ Vision loss may occur without warning, highlighting the importance of regular eye examinations.
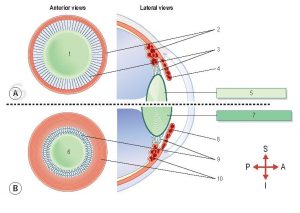
Stages of Diabetic Retinopathy
1. Non-Proliferative Diabetic Retinopathy (NPDR) This is the early stage of diabetic retinopathy.
Features:
Microaneurysms
Retinal hemorrhages
Hard exudates
Cotton wool spots
Retinal edema
Severity levels:
Mild NPDR
Moderate NPDR
Severe NPDR
2. Proliferative Diabetic Retinopathy (PDR)
This is the advanced and vision-threatening stage.
Features:
Neovascularization (new fragile blood vessels)
Vitreous hemorrhage
Fibrous tissue formation
Tractional retinal detachment
Neovascular glaucoma
Diabetic Macular Edema (DME)
Can occur at any stage
Involves swelling of the macula (central retina)
Leading cause of vision loss in diabetic patients
Diagnosis
Fundus examination
Fundus photography
Optical coherence tomography (OCT)
Fundus fluorescein angiography (FFA)
Prevention and Control
Strict blood sugar control
Control of blood pressure and lipids
Regular eye check-ups (annually or more often if advised)
Early treatment with laser, intravitreal injections, or surgery
Public Health Importance
Diabetic retinopathy is a major public health challenge due to the rising prevalence of diabetes. Early screening programs and patient education are essential to reduce blindness and socioeconomic burden.
Conclusion
Diabetic retinopathy is a serious yet largely preventable complication of diabetes that progressively damages the retina and can lead to irreversible vision loss if left untreated. It often remains asymptomatic in the early stages, making regular eye screening essential for all diabetic patients. Understanding its causes, recognizing symptoms early, and identifying the stages—from non- proliferative to proliferative diabetic retinopathy—are key to timely intervention. With strict control of blood sugar, blood pressure, and lipids, along with early diagnosis and appropriate treatment, most
cases of vision loss due to diabetic retinopathy can be effectively prevented, preserving sight and quality of life.