Introduction
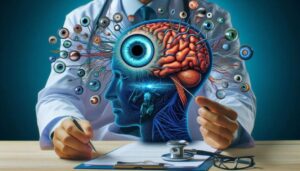
We all appreciate a sunny day, but the same rays that warm our skin and illuminate our surroundings also carry an unseen danger: ultraviolet (UV) radiation. While we often remember to use sunscreen for our skin, the fragile components of our eyes are just as, if not more, susceptible to the accumulating harm from UV exposure. Over time, this damage can result in various serious eye conditions, ranging from brief but uncomfortable ocular “sunburns” to irreversible vision impairment. The World Health Organization identifies solar UV radiation as a confirmed human carcinogen, highlighting the critical need for continuous protection.
This blog serves as a comprehensive guide to the top five eye conditions and diseases directly linked to UV radiation exposure. We will explore how UV rays affect different parts of the eye, what symptoms to watch for, and what treatments are available. Most importantly, we will discuss the simple, effective measures you can take to safeguard your vision. This information is intended for educational purposes and is not a substitute for professional medical advice. Always consult with your optometrist or ophthalmologist for a comprehensive eye examination and personalized recommendations for your eye health.
Eye Condition 1: Photokeratitis (Ultraviolet Keratitis)
Definition: Photokeratitis is a painful, acute inflammatory condition of the cornea—the clear front surface of the eye—caused by excessive exposure to UV radiation. It is often described as a “sunburn of the eye.”
Causes: This condition occurs after short-term, high-intensity exposure to UV rays, particularly UVB and UVC. The radiation is absorbed by the cornea’s outermost layer, the epithelium, causing widespread damage and death to the surface cells. Several hours after the exposure, these damaged cells slough off, exposing the highly sensitive corneal nerve endings beneath, which results in significant pain. Common sources of exposure include reflections from snow (often called “snow blindness”), sand, or water; artificial sources like welding arcs (“arc eye”), tanning beds, and improperly used germicidal lamps.
Symptoms: A key feature of photokeratitis is the delayed onset of symptoms, which typically appear 6 to 12 hours after the UV exposure. Patients often feel fine immediately after the activity, only to experience symptoms later. These include severe eye pain, a gritty or sandy sensation, intense sensitivity to light (photophobia), excessive tearing, redness, and blurred vision.
Diagnosis: An eye care professional diagnoses photokeratitis based on the patient’s history of recent UV exposure and a clinical examination. Using a slit-lamp microscope and fluorescein dye, the doctor can see a characteristic pattern of diffuse, tiny dots (punctate epithelial erosions) staining across the corneal surface, indicating where the epithelial cells have been damaged.
Treatment: Treatment is supportive, as the corneal epithelium has a remarkable ability to heal itself, typically within 24 to 72 hours. Management focuses on comfort and preventing secondary infection. This includes preservative-free artificial tears, lubricating antibiotic ointments, and oral pain relievers. Eye patching is generally not recommended as it does not improve healing rates.
Prevention: Photokeratitis is almost entirely preventable. Wearing properly fitting sunglasses that block 99-100% of UVA and UVB rays (often labeled “UV400”) is essential for recreational activities. For occupational hazards like welding, a full face shield that meets industry safety standards is required for adequate protection.
Eye Condition 2: Pterygium
Definition: A pterygium is a benign, raised, wedge-shaped growth of fibrous and vascular tissue that extends from the conjunctiva (the transparent membrane covering the white part of the eye) onto the cornea. It is often referred to as “surfer’s eye” because it is common in individuals who spend considerable time in sunny, windy environments.
Causes: Sustained, long-term exposure to UV radiation is the primary environmental risk factor for the development of a pterygium. The prevailing theory suggests that UV light damages the limbal stem cells located at the junction of the cornea and conjunctiva. These cells normally function as a barrier, preventing the conjunctiva from encroaching onto the clear cornea. When this barrier is compromised by UV damage, the conjunctival tissue can multiply and spread over the corneal surface. Pterygia are most prevalent in populations residing in the “pterygium belt,” an equatorial zone between 37 degrees north and south latitude, where UV intensity is highest.
Symptoms: Many pterygia do not cause any symptoms. However, they can lead to significant irritation, including redness, a gritty or foreign body sensation, itching, and dryness. If the pterygium grows large enough to obscure the central part of the cornea or distort its shape, it can induce astigmatism and result in substantial blurring of vision.
Diagnosis: A pterygium is diagnosed based on its distinctive appearance during a comprehensive eye examination using a slit-lamp microscope.
Treatment: For mild cases with minor irritation, treatment involves lubricating eye drops or ointments and sometimes a short course of steroid drops to reduce inflammation. Surgical removal is the only way to eliminate a pterygium. Surgery is typically advised if the growth threatens vision, causes persistent discomfort, or is aesthetically problematic. A significant challenge with pterygium surgery is the high rate of recurrence. Modern surgical techniques, such as excising the growth and covering the area with a conjunctival autograft (a piece of the patient’s own healthy conjunctiva), have significantly reduced recurrence rates.
Prevention: The most effective prevention strategy is minimizing UV exposure. This includes consistently wearing high-quality, UV400 sunglasses, particularly wraparound styles that block peripheral light. Wearing a wide-brimmed hat offers additional, crucial protection.
Eye Condition 3: Cataracts
Definition: A cataract is characterized by the clouding or loss of transparency in the eye’s natural lens, which is typically clear. This lens functions similarly to a camera lens, focusing light onto the retina at the back of the eye. When it becomes cloudy, it scatters light, resulting in blurred vision. While treatable, cataracts are the leading cause of blindness globally.
Causes: Although aging is the primary cause of cataracts, extensive exposure to UV radiation throughout life is a significant and preventable risk factor that accelerates their formation. The main mechanism involved is photo-oxidation. Specifically, UVA rays penetrate the cornea and are absorbed by the lens, generating highly reactive molecules known as reactive oxygen species (ROS). These ROS cause oxidative stress, which damages the delicate structural proteins (crystallins) and lipids within the lens, leading them to clump and lose transparency, thus forming an opacity. Epidemiological research indicates a strong correlation between UV exposure and the development of cortical cataracts, a type that first appears as whitish, wedge-shaped opacities on the lens’s outer edge.
Symptoms: Cataracts typically develop slowly and without pain. Common symptoms include a gradual blurring or dimming of vision, increased difficulty seeing at night, sensitivity to light and glare, the perception of “halos” around lights, a need for brighter illumination when reading, and colors appearing faded or yellowish.
Diagnosis: Cataracts are diagnosed through a comprehensive eye examination with dilated pupils. An eye care professional uses a slit-lamp microscope to examine the lens, identify the type of cataract, and assess its severity.
Treatment: In the initial stages, vision may be improved with new eyeglasses, anti-glare sunglasses, or brighter lighting. However, the only effective treatment to restore vision is surgery. Cataract surgery involves removing the clouded natural lens and replacing it with a clear, artificial intraocular lens (IOL).
Prevention: Lifelong protection from UV radiation is a crucial strategy to postpone the onset and slow the progression of cataracts. This includes wearing UV400 sunglasses and a wide-brimmed hat whenever outdoors, regardless of the season or cloud cover.
Eye Condition 4: Age-Related Macular Degeneration (AMD)
Definition: Age-related macular degeneration (AMD) is a chronic, progressive condition impacting the macula, the small central part of the retina crucial for sharp, detailed, straight-ahead vision. It is a primary cause of irreversible vision loss in individuals over 50.
Causes: The link between UV light and AMD is more intricate and debated compared to cataracts or pterygium. The eye’s natural structures, the cornea and lens, absorb almost all UV radiation, offering substantial protection to the retina. However, a part of the solar spectrum called high-energy visible (HEV) light, or “blue light” (wavelengths 400-500 nm), does reach the retina. This light is thought to cause significant photochemical damage and oxidative stress in the retinal pigment epithelium (RPE) and photoreceptor cells. While blue light is considered a main contributor, prolonged UV exposure is believed to add to the cumulative lifetime oxidative stress that underlies AMD’s development and progression.
Symptoms: AMD affects central vision while preserving peripheral vision. Symptoms can include a gradual or sudden blurring of central vision, distortion of straight lines (metamorphopsia), or the appearance of a dark or empty area in the center of vision (a central scotoma).
Diagnosis: AMD is diagnosed through a dilated eye exam. An eye care professional will look for characteristic signs like drusen (yellow deposits under the retina) and changes in the RPE. Advanced imaging techniques such as optical coherence tomography (OCT) are used to visualize retinal layers in detail and detect fluid leakage or atrophy.
Prevention: Protecting the eyes from intense sunlight (both UV and blue light) throughout life is a recommended preventive approach. Other vital measures include not smoking, maintaining a healthy weight, and eating a diet rich in antioxidants, especially leafy green vegetables and fish.
Eye Condition 5: Cancers of the Eyelid
Definition: These are malignant growths that develop from the skin of the eyelids. The eyelid skin is the thinnest on the body, making it particularly susceptible to sun damage. About 90% of eyelid cancers are basal cell carcinomas (BCC), a slow-growing cancer that rarely spreads. Approximately 5-10% are squamous cell carcinomas (SCC), which have a higher likelihood of spreading. Melanoma of the eyelid is significantly less common.
Causes: The primary cause of eyelid skin cancers is prolonged exposure to UV radiation from the sun. UV rays directly damage the DNA within skin cells, leading to genetic mutations that can cause uncontrolled cell growth. The lower eyelid is the most frequent site for these cancers, accounting for the majority of cases, as its orientation receives the most direct and extended sun exposure.
Symptoms: The warning signs of eyelid cancer can be subtle. They include a firm, painless, pearly or waxy bump; a flat, scaly patch; a sore that repeatedly bleeds, crusts over, and does not heal; or the unexplained loss of eyelashes.
Diagnosis: If a suspicious lesion is found, a biopsy is performed. A small tissue sample is removed and examined under a microscope to confirm the cancer diagnosis.
Treatment: The most effective treatment for most non-melanoma eyelid cancers is Mohs micrographic surgery. This precise technique involves removing the tumor one thin layer at a time and microscopically examining each layer until no cancer cells remain. This method maximizes the cure rate while preserving the greatest amount of healthy tissue, which is crucial for maintaining the function and cosmetic appearance of the delicate eyelid area.
Prevention: Diligent sun protection is essential. This includes wearing wide-brimmed hats and wraparound sunglasses that offer excellent coverage for the eyelids and surrounding skin. It is also important to apply a broad-spectrum sunscreen with an SPF of 30 or higher to the face, being careful to cover the skin around the eyes.
Conclusion
The evidence is clear: unprotected exposure to ultraviolet radiation poses a significant and multifaceted threat to our long-term vision and eye health. From the acute, searing pain of photokeratitis to the slow, insidious development of cataracts, macular degeneration, and eyelid cancers, the damage is cumulative and often irreversible.
The good news is that nearly all of these conditions are highly preventable. By taking proactive and consistent steps, you can drastically reduce your lifetime risk. Make it a habit to wear high-quality, UV400 sunglasses and a wide-brimmed hat every time you are outdoors. Be mindful of peak sun hours and reflective surfaces like snow and water. Most importantly, schedule regular comprehensive eye examinations with your optometrist. These exams are crucial for detecting the early, often silent, signs of sun damage, allowing for timely intervention that can protect your precious sight for years to come.
References
Izadi, M., Jonaidi-Jafari, N., Pourazizi, M., Alemzadeh-Ansari, M. H., & Hoseinpourfard, M. J. (2018). Photokeratitis induced by ultraviolet radiation in travelers: A major health problem. Journal of Postgraduate Medicine, 64(1), 40–46. https://doi.org/10.4103/jpgm.JPGM_52_17
Moran, D. J., & Hollows, F. C. (1984). Pterygium and ultraviolet radiation: a positive correlation. British Journal of Ophthalmology, 68(5), 343–346. https://doi.org/10.1136/bjo.68.5.343
Delcourt, C., Cougnard-Grégoire, A., Boniol, M., Carrière, I., Doré, J. F., Delyfer, M. N., Rougier, M. B., Le Goff, M., Dartigues, J. F., Barberger-Gateau, P., & Korobelnik, J. F. (2014). Lifetime exposure to ambient ultraviolet radiation and the risk for cataract extraction and age-related macular degeneration: The ALIENOR study. Investigative Ophthalmology & Visual Science, 55(11), 7619–7627. https://doi.org/10.1167/iovs.14-14471
Chalam, K. V., Khetpal, V., Rusovici, R., & Balaiya, S. (2011). A review: role of ultraviolet radiation in age-related macular degeneration. Eye & Contact Lens, 37(4), 225–232. https://doi.org/10.1097/ICL.0b013e31821fbd3e
Fan, W., Rokohl, A. C., Guo, Y., Chen, H., Gao, T., Kakkassery, V., & Heindl, L. M. (2023). Narrative review: mechanism of ultraviolet radiation-induced basal cell carcinoma. Frontiers of Oral and Maxillofacial Medicine, 5, 9. https://doi.org/10.21037/fomm-21-31